i-Virtual develops its solutions around a technology that uses light – photoplethysmography. In “photoplethysmography”, there is the Greek word photo that refers to light and the word plethysmo that means “enlargement”, “increase”. Introduced in the 1930s, this term was suggested to represent the volumetric changes in the dermal vasculature. But, what is photoplethysmography and how does it work?
Photoplethysmography: from contact to non contact
Photoplethysmography is a non-invasive optical technique for sensing microvascular blood volume changes in tissues which are due to the pulsatile nature of the circulatory system. It became an attractive area of research in the biomedical and clinical fields due to its ease of use, low cost, and convenience. Usually, there are two main ways of using this technique: contact and noncontact method.
Contact photoplethysmography
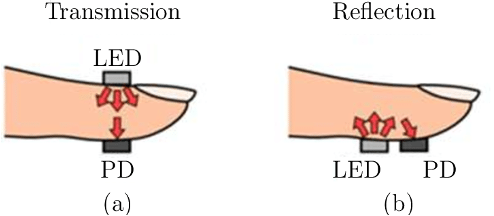
Contact photoplethysmography techniques relies on the light reflectance or transmission (two main PPG operational configurations). Fundamental principle of photoplethysmography relies on the variations in the sensitivity of different optical wavelengths for blood and other tissue components. Thus, basic form of PPG technology requires only a few optoelectronic components:
- A light source to illuminate the tissue
- A photodetector to measure the small variations in light intensity associated with changes in perfusion in the catchment volume.
In the transmission mode, the tissue sample is between the light source and the detector (Figure 1 (a)). While in the reflecting mode, the source of light and the detector are placed side by side (Figure 1 (b)).
For accurate monitoring of blood volume changes in the microvascular tissue bed, the light source, more precisely the wavelength, should have greater absorption for blood compared to other tissue components. Melanin strongly absorbs shorter wavelengths of light, while water absorbs light in the ultraviolet and longer infrared ranges. Consequently, red and near IR light are usually used as light sources in PPG sensors. However, more and more devices started to use green wavelength as the haemoglobin and the oxyhaemoglobin absorb green light better than red. This resulting in better signal with less noise.
The most common measurement sites for contact recording are fingers, forehead, wrist and ears.
Noncontact recordings
Noncontact photoplethysmography, or remote photoplethysmography, is part of imaging photoplethysmography (IPPG). Noncontact IPPG technique is a non-invasive optical method for detecting heart generated pulse waves by means of peripheral blood perfusion measurements. It has been proven to be superior in its ease of use, low cost, safe, convenience, and able to offer multiple physiological assessments.
Remote photoplethysmography has been explored relatively recently, since 1996. The basic concept of IPPG relies on the illumination of a specific tissue with a light source and then in the measurement of the light leaving the tissue with an imaging sensor. Thus, IPPG avoids the deformation of the atrial wall which gives more reliable signals for clinical applications.
Remote IPPG technique is relatively recent, but it spreads rapidly from lab to everyday use. Scientists and researchers focus mainly on the light source design and the control circuit development for synchronization between the light source and the camera. The second focus is done on the data processing. Especially because remote sensing approaches are known to be more vulnerable to motion artifacts.
Similarities and differences
PPG and IPPG applications
The use of PPG has important implications for a wide range of applications in different clinical settings, including cardiovascular system assessment, vital sign monitoring, blood oxygen detection and autonomic function. The PPG contact technique has been used in lots of commercially available medical devices for measuring oxygen saturation (SpO2), blood pressure and cardiac output, assessing autonomic function and detecting peripheral vascular disease.
Caducy and photoplethysmography
Today, devices using IPPG technique such can measure someone’s heart rate, respiration rate, blood oxygenation, pulse rate variability, blood perfusion, blood pressure, pulse transit time, detect atrial fibrillation and systolic and diastolic peaks. Caducy, developed by i-Virtual is a great example of the application of this technology. In fact, today, thank to Caducy, people’s heart rate, respiration rate, heart rate variability and stress level can be measured remotely using noncontact imaging photoplethysmography.